1- HBOT increases Stem Cell Growth
According to a study to be published in the American Journal of Physiology-Heart and Circulation Physiology, a typical course of hyperbaric oxygen treatments increases by eight-fold the number of stem cells circulating in a patient's body.

Stem cells, also called progenitor cells are crucial to injury repair.
Stem cells exist in the bone marrow of human beings and animals and are capable of changing their nature to become part of many different organs and tissues. In response to injury, these cells move from the bone marrow to the injured sites, where they differentiate into cells that assist in the healing process. The movement, or mobilization, of stem cells can be triggered by a variety of stimuli -- including pharmaceutical agents and hyperbaric oxygen treatments. Where as drugs are associated with a host of side effects, hyperbaric oxygen treatments carry a significantly lower risk of such effects. "This is the safest way clinically to increase stem cell circulation, far safer than any of the pharmaceutical options," said Stephen Thom, MD, Ph.D., Professor of Emergency Medicine at the University of Pennsylvania School of Medicine and lead author of the study. "This study provides information on the fundamental mechanisms for hyperbaric oxygen and offers a new theoretical therapeutic option for mobilizing stem cells." (Sciencedaily.com).
ONLY MEDICAL HBOT IS PROVEN TO PRODUCE THESE EFFECTS. The study was conducted in steel, medical chambers at pressures greater than 1.5ATA (2.0ATA to be exact) which is at least 32 feet of sea water. Many inflatable hyperbaric manufacturers and clinics are touting this exciting breakthrough without the means of ever replicating it. PLEASE view the study details below as published in the American Journal of Physiology – Heart and Circulation Physiology to see the details of the treatment.
2- HBOT significantly reduces swelling
Dilation or blood vessel widening following damage to tissue results in decreased blood flow. That increase in blood flow couples with vascular permeability (movement of fluid in and out of blood vessels) to increase protein and fluids outside blood vessels reducing tissue swelling. HBOT significantly reduces swelling, and reduces the pain associated with it. As the oxygen supply reduces, blood flow increases which will only serve to exacerbate the swelling and impede the inflammatory process that assists the commencement of healing.
Hyperbaric oxygen therapy reduces vascular vasodilation and permeability by increasing the oxygen content within the blood.
3- HBOT significantly reduces edema
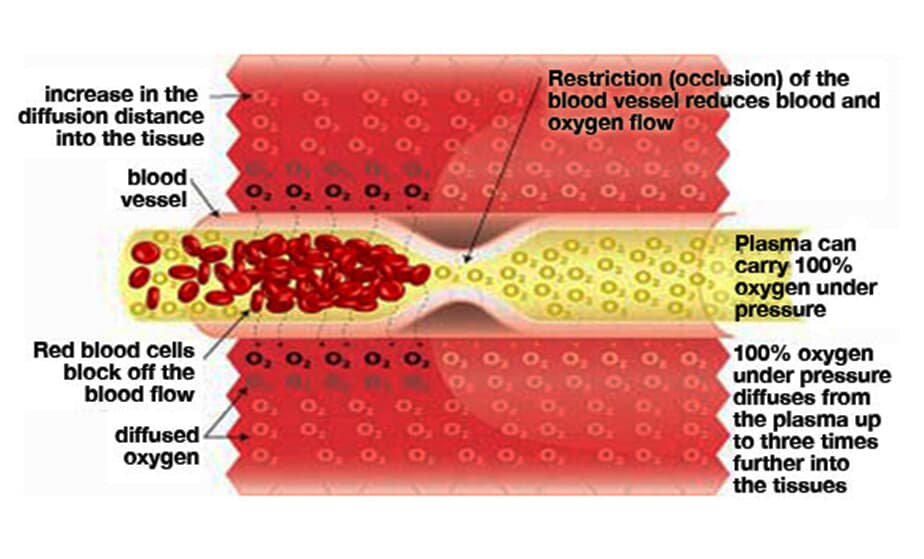
The development of edema (swelling) is caused by a number of factors such as an increase in local blood flow and also damage to local blood and lymphatic vessels. The pressure exerted by edema on surrounding structures can compromise circulation. When this pressure approaches or exceeds that in the blood vessels, then blood flow will slow or cease altogether. Swelling also contributes to tissue hypoxia (a shortage of oxygen in the tissues) by increasing the distance between the capillary (smallest blood vessels) and the cells, which impedes cell function, metabolism and the inflammatory process by increasing the diffusion distance (movement of particles from an area of high concentration to an area of low concentration).
Hyperbaric oxygen therapy is able to combat the increased distance for oxygen diffusion from blood vessel to cells by increasing the oxygen content within the blood which will result in an increased oxygen delivery to cells and tissues, shortening the inflammatory process, thereby speeding the healing and repair of tissues.
4- HBOT significantly shortens the inflammatory process
The bodies initial response to any injury involves inflammation. Inflammation is the process by which cells such as phagocytes (white blood cells) gain access to the damaged/injured tissues to prevent infection and enable healing to commence. Decreased oxygen supply greatly impacts the inflammatory process as the cells involved in inflammation are oxygen dependent. Should oxygen supply be decreased, the inflammatory process and healing will be impaired.
Increased oxygen availability promotes vasoconstriction when blood vessels in the body become smaller which causes fluid reabsorption and helps reduce edema while keeping the tissue well oxygenated. This supports the cells of the inflammatory process in removing cell debris and micro-organisms that impede infection. White blood cells have an increase in cellular energy that speeds up their activity and reduces the time of the inflammatory process.
5- HBOT improves range of motion
Following hyperbaric oxygen therapy, swelling is also decreased and resolved more rapidly. As a result, pain will be less allowing for the return of range of motion as the healing process gains momentum and inflammation is decreased.
6- HBOT increases the production of collagen
Following the initial healing process of the inflammatory response and the prevention or removal of infection, comes the next chapter in tissue/wound healing. Collagen is the connective tissue developed and laid down by fibroblasts, the repair cells of the body. Collagen acts as a base layer in the healing wound and assists the wound to close and repair. The formation of collagen and hence wound healing/recovery is highly dependent on the presence of adequate amounts of oxygen. The actual production of collagen by fibroblasts is also extremely dependent on oxygen availability.
As hyperbaric oxygen therapy markedly increases the oxygen available within the blood this in turn enables for a cross-linking or strengthening of the tissues, and fibroblasts to produce increased amounts of collagen required for healing of wounds and tissue damage.
7- HBOT increases growth of cells that form reparative tissue (Fibroblastic proliferation)
Clinical research has demonstrated that a number of days following injury there occurs a migration of fibroblasts (connective tissue cells responsible for collagen production) into the area of damage. These cells then divide and replicate producing large amounts of collagen (connective tissue used to repair damage to tissue) that acts as the building block for the healing of tissue and wounds.
The development and migration of fibroblasts is assisted by the influx of oxygen resulting from hyperbaric oxygen therapy, this then supports the development and action of these particular cells which play a vital part in the healing/recovery process.
8- HBOT supports scar tissue rehabilitation
A decrease in oxygen available to cells such as fibroblasts impairs their action, impacting upon the healing of tissue, causing healing to take longer, and inhibiting the quality of scar tissue developed or rehabilitated, which in turn greatly decreases tissue strength.
Healing occurs both faster and stronger in wounds/injuries that are treated with hyperbaric oxygen therapy due to the demands of oxygen availability by the cells and tissues responsible for the healing process being met.
9- HBOT promotes greater tissue strength
As the oxygen concentration of the blood increases during hyperbaric oxygen therapy, cells further from blood vessels are more adequately oxygenated. Hyperbaric oxygen therapy allows for increased oxygen availability in more extensive areas enabling fibroblasts to carry out their part of the healing process for tissue damage and injury, more rapidly covering larger areas.
Hyperbaric oxygen therapy saturates the blood plasma with oxygen, this in turn reaches the areas of damage/injury with greater efficiency than red blood cells, providing all cells and tissues with the much needed agent for healing, oxygen. The cells responsible for the development of scar tissue for healing are then able to carry this out more rapidly and the resulting tissue integrity is stronger.
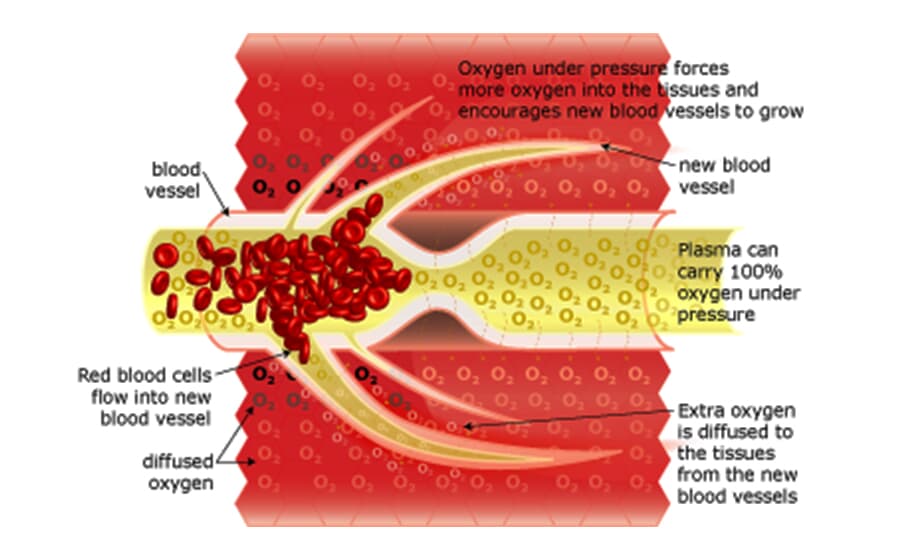
10- HBOT enhances the growth of new blood vessels (Angiogenesis)
Injury or damage to tissues also results in damage and destruction of the supporting blood vessel structures. The healing process is reliant on these structures for supply of the blood containing the cells and nutrients that carry out and enable healing as well as the removal of damaged cells, debris and foreign micro-organisms.
Research has demonstrated that treatment with hyperbaric oxygen therapy significantly increases the number and actual size of blood vessels in damaged tissues and wounds. This allows the healing process to occur faster speeding the recovery of the injury or wound.
11- HBOT increases oxygen levels in tissues (Hyperoxia)
With an increase in oxygen availability resulting from both blood that is highly saturated in oxygen dissolved in the plasma, and an increase in the number of blood vessels due to new vessels being created as well as the healing of damaged blood vessels, tissues and cells become highly saturated in oxygen.
12- HBOT increases oxygen perfusion area around wounds
Oxygen perfusion around wounds and damaged tissues is greatly increased when the blood supply to these areas possesses greater than normal levels of oxygen within blood plasma as well as carried on red blood cells. The oxygen contained in the blood plasma is more easily accessible than that carried to the tissues and cells of the wound/damaged area on red blood cells, and this method of oxygen supply is less labor intensive and energy taxing.
The cells involved in the healing process are highly dependent on oxygen to carry out their healing function and this increased demand for oxygen in the area around wounds by the increased number of healing cells in that location is met by the increased oxygen saturation of the blood following hyperbaric oxygen therapy.
13- HBOT stimulates new capillary growth
During the time of injury and damage the microcirculation and the blood vessels of this circulation (capillaries) are vital to the healing process through the supply of nutrients and oxygen and the removal of waste and debris to enable the cells responsible for healing to successfully complete their function.
Growth of new, and repair of damaged capillaries are stimulated within the damaged tissues by hyperbaric oxygen therapy, providing increased oxygen availability to these areas. The increased oxygen supply and increased pressure employed by hyperbaric oxygen supply are both responsible for the stimulation of new capillary growth and the repair of existing capillaries.
14- HBOT improves the survival of tissues in the 'grey area' of crush injuries
The 'grey area' of crush injuries can be defined as the area between the tissues that are obviously irreversibly damaged and those tissues that are undamaged. The tissues of the 'grey area' benefit greatly from increased oxygen supply, improved circulation and blood supply. These are the aspects that will allow the tissues of the 'grey area' to be saved, salvaged and repaired.
Hyperbaric oxygen therapy has been shown to support and maintain tissue oxygenation within the 'grey area' resulting in a better outcome for the tissues, wound or injury.
15- HBOT increases production and improves the action of Osteoblasts and Osteoclasts
Osteoblasts are the cells responsible for bone formation and osteoclasts are the cells responsible for bone reabsorption. Both these cells work together to form bones and control the amount of bone tissue.
The provision of increased levels of oxygen allows for increased production of these cells and enables them to conduct bone repair and formation more adequately through the reduction of edema and growth of new blood vessels in the micro-circulation.
16- HBOT improves bone regeneration for faster recovery
When the inflammatory process, swelling and edema is rectified more rapidly the repair and regeneration of bone is able to commence sooner.
With the increase in blood supply and oxygen availability, the tissues and cells responsible for bone regeneration are able to carry out their task of healing more efficiently, resulting in accelerated recovery and a better result in the healing tissues.
17- HBOT helps prevent infection
Research has demonstrated that having lower oxygen levels in tissues and wounds increases the possibility of infection. Changes in wound and tissue oxygenation impacts greatly upon the wound immune mechanism.
Having an improved or increased tissue oxygen supply reduces the incidence of wound infection as the cells responsible for prevention and recovery from infection are dependent on oxygen, therefore additional oxygen benefits the healing process.
18- HBOT increases white blood cell production
The major players in the bodies immune response are the white blood cells. Providing the body with increased oxygen availability increases the production of white blood cells providing benefit to the bodies immune response.
High-dose oxygen delivered under pressures greater than sea level (hyperbaric oxygen therapy), stimulates and enables the bodies immune response.
19- HBOT enhances ability of white blood cells to remove bacteria and debris (Leukocyte activity)
Without oxygen or in a hypoxic (shortage of oxygen in the body) environment the function of white blood cells becomes diminished. This in turn provides a significant threat of infection as the bodies immune response is impaired.
The increased oxygen supply offered by hyperbaric oxygen therapy assists in bacterial killing through improving leukocyte (type of white blood cell) function.
20- HBOT potentiates the use of antibiotics
Research has demonstrated that periods of hyperoxia (increased oxygen levels in tissues) and hyperbaric oxygen therapy has influenced the activity of some antibiotics, enhancing their effectiveness. This enables the presenting infection to resolve quicker.
21- HBOT destroys harmful bacteria (Antimicrobial effect)
Hyperbaric oxygen therapy provides direct bactericidal (substance that kills bacteria) and bacteriostatic (hampers the growth of bacteria) effects against bacteria due to the generation of oxygen free radicals. These free radicals are able to damage the membranes and make up of the bacteria rendering them ineffective or killing them. Anaerobic (without oxygen) organisms find an increased oxygen environment toxic and are unable to survive.
22- Hyperbaric Oxygenation Effects the Blood Flow
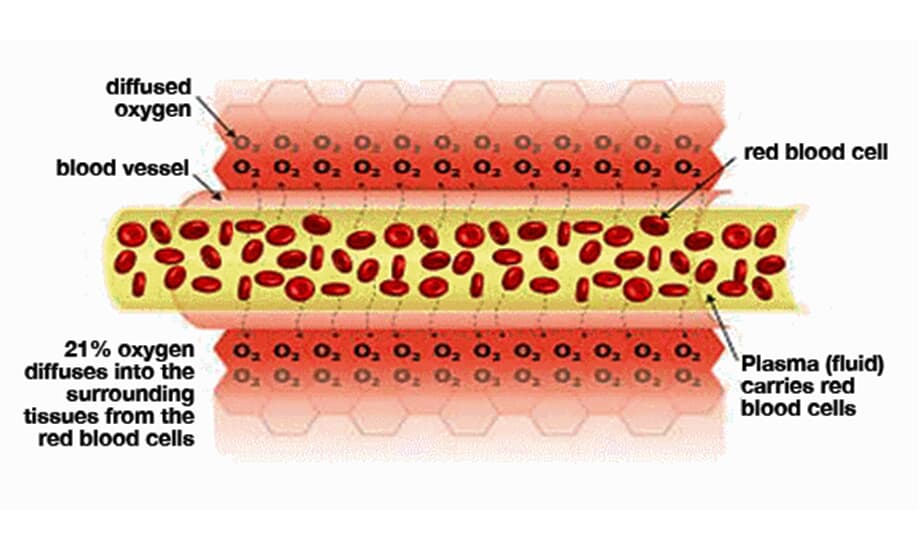
Normal blood flow There is 21% oxygen in the air that we breathe, and our lungs transfer this oxygen to our red blood cells (via hemoglobin). These oxygen-filled red blood cells are carried around the body by the plasma (fluid), which travels through the blood vessels. The oxygen diffuses into the surrounding tissue ensuring that it is delivered to where it is needed most.
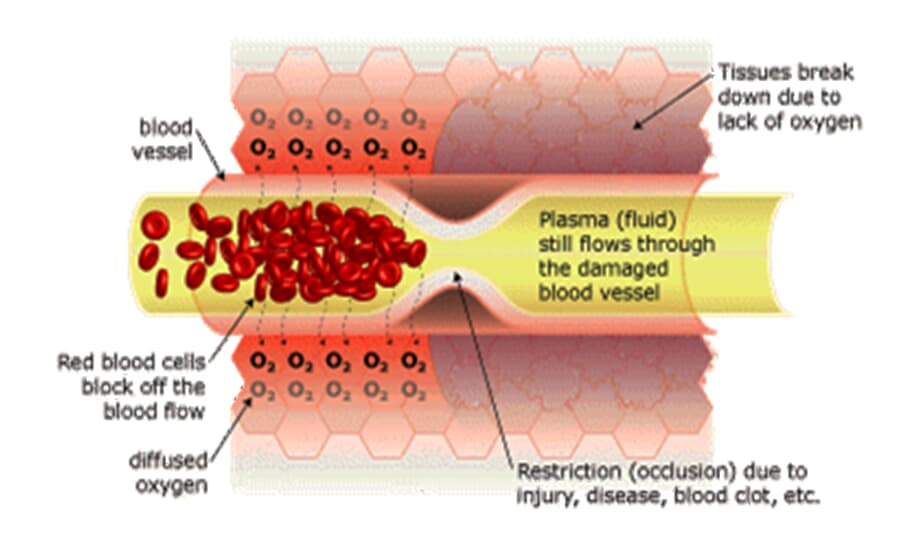
Restricted blood flow (ischemia) causes Hypoxia When there is a restriction (occlusion) in blood flow due to surgery, illness, or injury, the red blood cells block the blood vessel and are unable to transfer oxygen to the cells on the other side of the occlusion. This causes swelling and starves the area of oxygen, causing hypoxia (a lack of oxygen); when this occurs the tissue begins to break down. Hypoxia triggers ‘apoptosis’ (programmed cellular degeneration – clumping and clustering of damaged nerve cells surrounded by healthy neuronal tracts). Apoptosis modifies the expression of plasticity (the ability of the body to repair). Apoptotic bodies and altered DNA fragmentations are observed in the avascular ischemic region with increased inhibitory biochemical factors (proteins) released into the damaged parts of the brain and spinal cord causing further deterioration. Apoptosis has been identified in all neurodegenerative disorders including brain and spinal cord injury. Apoptosis fosters the cycle of continued dysfunction, degeneration and ultimate neuronal death.
Hyperbaric Oxygenation Breathing 100% oxygen under pressure causes the oxygen to diffuse into the blood plasma. This oxygen-rich plasma is able to travel past the restriction, diffusing up to 3 times further into the tissue. The pressurized environment helps to reduce swelling and discomfort, while providing the body with at least 10-15 times its normal supply of oxygen to help repair tissue damaged by the original occlusion or subsequent hypoxic condition. Hyperbaric Oxygenation (HBOT) directly increases the saturation of tissue oxygenation, slowing and reversing hypoxic induced apoptosis - restoring blood supply to the compromised region by the development of new capillary networks (neovascularization) enabling the body to alter the course and impact of the disease process.
Neurovascular Regeneration HBOT mobilizes the body’s circulating stem cells. American Journal Physiology - Heart and Circulatory Physiology (Nov 05)] reports a single 2-hour exposure to HBOT at 2 ATA doubles circulating CD34+ progenitor stem cells (primordial cells targeted to salvage and restore damaged structures); and at approx. 40-hours of HBOT; circulating CD34+ cells increases eight fold (800%).